PAHP is now offering Telehealth & Virtual Visits!
VDH’s Return to School Guidance, Sept. 2022
COVID Vaccine Checklist for Kids
COVID Vaccines for Kids 6 Months & Older: FAQs for Families
What should parents know about the COVID vaccine for kids under 5?
When can kids get the COVID vaccine or booster?
COVID-19 Patient Education
January 10, 2022
CDC Updates and Shortens Recommended Isolation and Quarantine Period
January 3, 2022
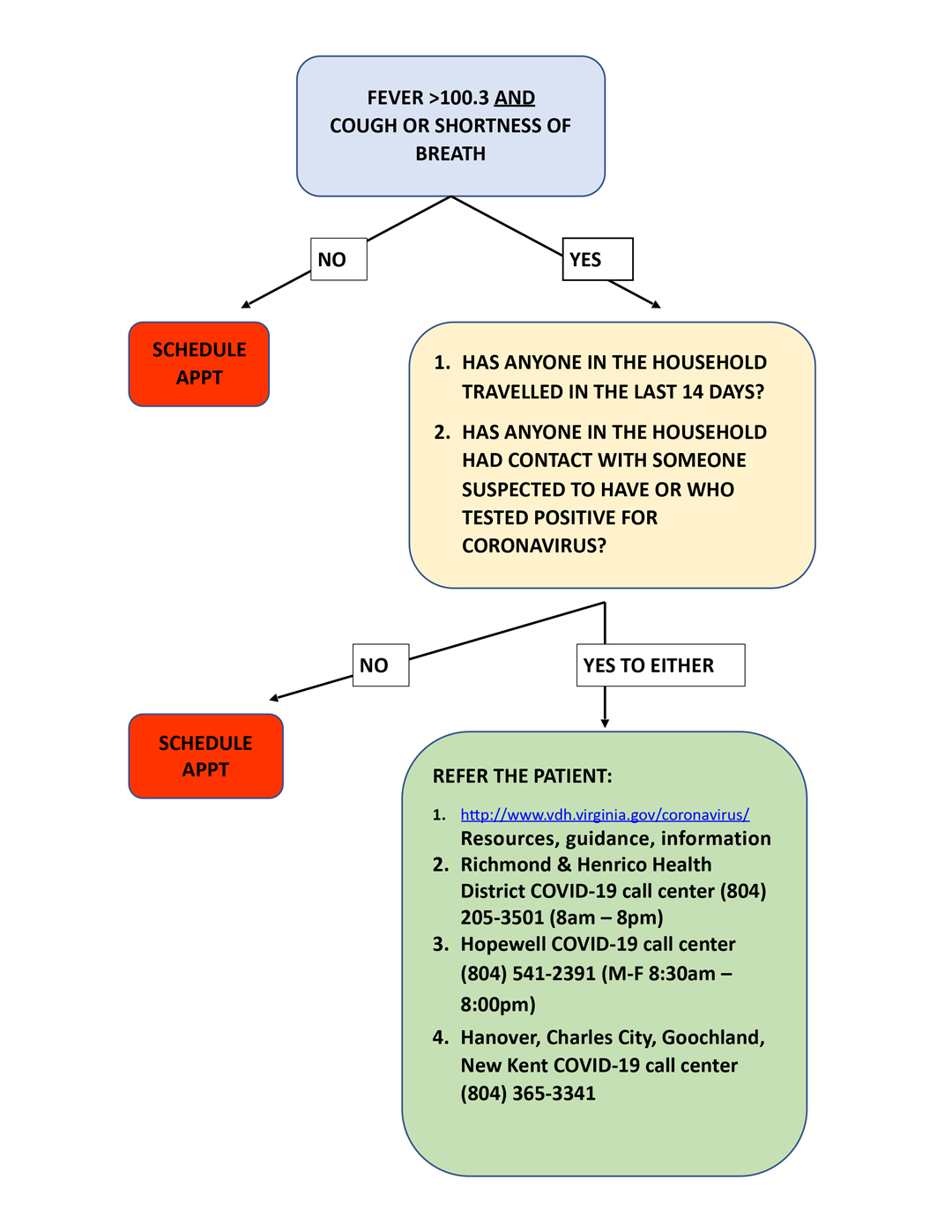
VDH Algorithm for Evaluating a Child with COVID-19 Symptoms or Exposure
December 22, 2020
Protect your home from COVID-19
December 1, 2020
CDC Toolkit for Youth Sports
October 28, 2020
8 Things to Know about Vaccine Planning
October 20, 2020
Latest version of VDH’s return to school guidance
October 10, 2020
After You Travel
September 22, 2020
Data on COVID-19 during Pregnancy
September 14, 2020
What CDC Is Doing About Multisystem Inflammatory Syndrome in Children (MIS-C)
September 9, 2020
Coronavirus (COVID-19) Diagnosed or Suspected Related Symptoms: definitions, who to call and care advice
September 4, 2020
Duration of Isolation and Precautions for Adults with COVID-19
August 17, 2020
CDC Expects 2020 Outbreak of Life-Threatening Acute Flaccid Myelitis
August 7, 2020
Toolkit for K-12
August 3, 2020
Returning To Play After Coronavirus Infection: Pediatric Cardiologists’ Perspective
July 28, 2020
CDC Launches Natural Disasters and COVID-19 Response Website
July 16, 2020
Toolkit for Young Adults, 15-21
July 15, 2020
Caring for Children with Asthma During COVID-19: Parent FAQs
July 9, 2020
FREE Community COVID-19 Testing
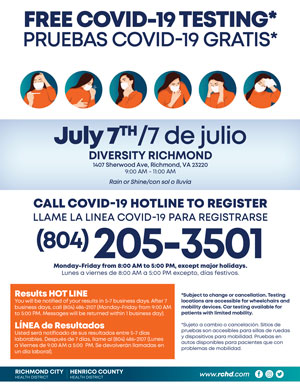
July 3, 2020
Considerations for Travelers – Coronavirus in the US
June 25, 2020
Food and Coronavirus Disease 2019 (COVID-19)
June 22, 2020
CDC releases new guidance for staying safe from COVID-19 as communities re-open
June 15, 2020
Vaccine Guidance During A Pandemic
Read on cdc.gov
June 10, 2020
Routine vaccination is an essential preventive care service for children, adolescents, and adults (including pregnant women) that should not be delayed because of the COVID-19 pandemic. In light of COVID-19-related reductions in people accessing vaccination services, it is important to assess the vaccination status of all children and adolescents at each patient visit to avoid missed opportunities for vaccination and ensure timely vaccine catch-up. All vaccines due or overdue should be administered according to the recommended CDC immunization schedules during that visit, unless a specific contraindication exists, to provide protection as soon as possible as well as minimize the number of healthcare visits needed to complete vaccination.
When You Can be Around Others After You Had or Likely Had COVID-19
May 28, 2020
When you can be around others (end home isolation) depends on different factors for different situations. Find CDC’s recommendations for your situation below.
I think or know I had COVID-19, and I had symptoms
You can be with others after
- 3 days with no fever and
- Symptoms improved and
- 10 days since symptoms first appeared
I tested positive for COVID-19 but had no symptoms
If you continue to have no symptoms, you can be with others after:
- 10 days have passed since test
Depending on your healthcare provider’s advice and availability of testing, you might get tested to see if you still have COVID-19. If you will be tested, you can be around others after you receive two negative test results in a row, at least 24 hours apart.
If you develop symptoms after testing positive, follow the guidance above for “I think or know I had COVID, and I had symptoms.”
I have a weakened immune system (immunocompromised) due to a health condition or medication. When can I be around others?
People with conditions that weaken their immune system might need to stay home longer than 10 days. Talk to your healthcare provider for more information. If testing is available in your community, it may be recommended by your healthcare provider. You can be with others after you receive two negative test results in a row, at least 24 hours apart.
If testing is not available in your area, your doctor should work with an infectious disease expert at your local health department to determine if you are likely to spread COVID-19 to others and need to stay home longer.
For Anyone Who Has Been Around a Person with COVID-19
It is important to remember that anyone who has close contact with someone with COVID-19 should stay home for 14 days after exposure based on the time it takes to develop illness.
Read on cdc.gov
Considerations for Schools
May 21, 2020
As some communities in the United States open K-12 schools, CDC offers the following considerations for ways in which schools can help protect students, teachers, administrators, and staff and slow the spread of COVID-19. Schools can determine, in collaboration with state and local health officials to the extent possible, whether and how to implement these considerations while adjusting to meet the unique needs and circumstances of the local community. Implementation should be guided by what is feasible, practical, acceptable, and tailored to the needs of each community. School-based health facilities may refer to CDC’s Guidance for U.S. Healthcare Facilities and may find it helpful to reference the Ten Ways Healthcare Systems Can Operate Effectively During the COVID-19 Pandemic. These considerations are meant to supplement—not replace—any state, local, territorial, or tribal health and safety laws, rules, and regulations with which schools must comply.
Guiding Principles to Keep in Mind
The more people a student or staff member interacts with, and the longer that interaction, the higher the risk of COVID-19 spread. The risk of COVID-19 spread increases in school settings as follows:
- Lowest Risk: Students and teachers engage in virtual-only classes, activities, and events.
- More Risk: Small, in-person classes, activities, and events. Groups of students stay together and with the same teacher throughout/across school days and groups do not mix. Students remain at least 6 feet apart and do not share objects (e.g., hybrid virtual and in-person class structures, or staggered/rotated scheduling to accommodate smaller class sizes).
- Highest Risk: Full sized, in-person classes, activities, and events. Students are not spaced apart, share classroom materials or supplies, and mix between classes and activities.
COVID-19 is mostly spread by respiratory droplets released when people talk, cough, or sneeze. It is thought that the virus may spread to hands from a contaminated surface and then to the nose or mouth, causing infection. Therefore, personal prevention practices (such as handwashing, staying home when sick) and environmental cleaning and disinfection are important principles that are covered in this document. Fortunately, there are a number of actions school administrators can take to help lower the risk of COVID-19 exposure and spread during school sessions and activities.
Promoting Behaviors that Reduce Spread
Schools may consider implementing several strategies to encourage behaviors that reduce the spread of COVID-19.
- Staying Home when Appropriate
- Educate staff and families about when they/their child(ren) should stay home and when they can return to school.
- Actively encourage employees and students who are sick or who have recently had close contact with a person with COVID-19 to stay home. Develop policies that encourage sick employees and students to stay at home without fear of reprisal, and ensure employees, students, and students’ families are aware of these policies. Consider not having perfect attendance awards, not assessing schools based on absenteeism, and offering virtual learning and telework options, if feasible.
- Staff and students should stay home if they have tested positive for or are showing COVID-19 symptoms.
- Staff and students who have recently had close contact with a person with COVID-19 should also stay home and monitor their health.
- CDC’s criteria can help inform when employees should return to work:
- Hand Hygiene and Respiratory Etiquette
- Teach and reinforce handwashing with soap and water for at least 20 seconds and increase monitoring to ensure adherence among students and staff.
- If soap and water are not readily available, hand sanitizer that contains at least 60% alcohol can be used (for staff and older children who can safely use hand sanitizer).
- Encourage staff and students to cover coughs and sneezes with a tissue. Used tissues should be thrown in the trash and hands washed immediately with soap and water for at least 20 seconds.
- If soap and water are not readily available, hand sanitizer that contains at least 60% alcohol can be used (for staff and older children who can safely use hand sanitizer).
- Teach and reinforce handwashing with soap and water for at least 20 seconds and increase monitoring to ensure adherence among students and staff.
- Cloth Face Coverings
- Teach and reinforce use of cloth face coverings. Face coverings may be challenging for students (especially younger students) to wear in all-day settings such as school. Face coverings should be worn by staff and students (particularly older students) as feasible, and are most essential in times when physical distancing is difficult. Individuals should be frequently reminded not to touch the face covering and to wash their hands frequently. Information should be provided to staff, students, and students’ families on proper use, removal, and washing of cloth face coverings.
- Note: Cloth face coverings should not be placed on:
- Children younger than 2 years old
- Anyone who has trouble breathing or is unconscious
- Anyone who is incapacitated or otherwise unable to remove the cloth face covering without assistance
- Note: Cloth face coverings should not be placed on:
- Cloth face coverings are meant to protect other people in case the wearer is unknowingly infected but does not have symptoms. Cloth face coverings are not surgical masks, respirators, or other medical personal protective equipment.
- Teach and reinforce use of cloth face coverings. Face coverings may be challenging for students (especially younger students) to wear in all-day settings such as school. Face coverings should be worn by staff and students (particularly older students) as feasible, and are most essential in times when physical distancing is difficult. Individuals should be frequently reminded not to touch the face covering and to wash their hands frequently. Information should be provided to staff, students, and students’ families on proper use, removal, and washing of cloth face coverings.
- Adequate Supplies
- Support healthy hygiene behaviors by providing adequate supplies, including soap, hand sanitizer with at least 60 percent alcohol (for staff and older children who can safely use hand sanitizer), paper towels, tissues, disinfectant wipes, cloth face coverings (as feasible) and no-touch/foot-pedal trash cans.
- Signs and Messages
- Post signs in highly visible locations (e.g., school entrances, restrooms) that promote everyday protective measurespdf icon and describe how to stop the spreadpdf icon of germs (such as by properly washing hands and properly wearing a cloth face coveringimage icon).
- Broadcast regular announcements on reducing the spread of COVID-19 on PA systems.
- Include messages (for example, videos) about behaviors that prevent the spread of COVID-19 when communicating with staff and families (such as on school websites, in emails, and on school social media accounts).
- Find free CDC print and digital resources on CDC’s communications resources main page.
Maintaining Healthy Environments
Schools may consider implementing several strategies to maintain healthy environments.
- Cleaning and Disinfection
- Clean and disinfect frequently touched surfaces (e.g., playground equipment, door handles, sink handles, drinking fountains) within the school and on school buses at least daily or between use as much as possible. Use of shared objects (e.g., gym or physical education equipment, art supplies, toys, games) should be limited when possible, or cleaned between use.
- If transport vehicles (e.g., buses) are used by the school, drivers should practice all safety actions and protocols as indicated for other staff (e.g., hand hygiene, cloth face coverings). To clean and disinfect school buses or other transport vehicles, see guidance for bus transit operators.
- Develop a schedule for increased, routine cleaning and disinfection.
- Ensure safe and correct use and storage of cleaning and disinfection productsexternal icon, including storing products securely away from children. Use products that meet EPA disinfection criteriaexternal icon.
- Cleaning products should not be used near children, and staff should ensure that there is adequate ventilation when using these products to prevent children or themselves from inhaling toxic fumes.
- Shared Objects
- Discourage sharing of items that are difficult to clean or disinfect.
- Keep each child’s belongings separated from others’ and in individually labeled containers, cubbies, or areas.
- Ensure adequate supplies to minimize sharing of high touch materials to the extent possible (e.g., assigning each student their own art supplies, equipment) or limit use of supplies and equipment by one group of children at a time and clean and disinfect between use.
- Avoid sharing electronic devices, toys, books, and other games or learning aids.
- Ventilation
- Ensure ventilation systems operate properly and increase circulation of outdoor air as much as possible, for example by opening windows and doors. Do not open windows and doors if doing so poses a safety or health risk (e.g., risk of falling, triggering asthma symptoms) to children using the facility.
- Water Systems
- To minimize the risk of Legionnaire’s disease and other diseases associated with water, take steps to ensure that all water systems and features (e.g., sink faucets, drinking fountains, decorative fountains) are safe to use after a prolonged facility shutdown. Drinking fountains should be cleaned and sanitized, but encourage staff and students to bring their own water to minimize use and touching of water fountains.
- Modified Layouts
- Space seating/desks at least 6 feet apart when feasible.
- Turn desks to face in the same direction (rather than facing each other), or have students sit on only one side of tables, spaced apart.
- Create distance between children on school buses (g., seat children one child per row, skip rows) when possible.
- Physical Barriers and Guides
- Install physical barriers, such as sneeze guards and partitions, particularly in areas where it is difficult for individuals to remain at least 6 feet apart (e.g., reception desks).
- Provide physical guides, such as tape on floors or sidewalks and signs on walls, to ensure that staff and children remain at least 6 feet apart in lines and at other times (e.g. guides for creating “one way routes” in hallways).
- Communal Spaces
- Close communal use shared spaces such as dining halls and playgrounds with shared playground equipment if possible; otherwise, stagger use and clean and disinfect between use.
- Add physical barriers, such as plastic flexible screens, between bathroom sinks especially when they cannot be at least 6 feet apart.
- Food Service
- Have children bring their own meals as feasible, or serve individually plated meals in classrooms instead of in a communal dining hall or cafeteria, while ensuring the safety of children with food allergies.pdf icon
- Use disposable food service items (e.g., utensils, dishes). If disposable items are not feasible or desirable, ensure that all non-disposable food service items are handled with gloves and washed with dish soap and hot water or in a dishwasher. Individuals should wash their hands after removing their gloves or after directly handling used food service items.
- If food is offered at any event, have pre-packaged boxes or bags for each attendee instead of a buffet or family-style meal. Avoid sharing food and utensils and ensure the safety of children with food allergies.pdf icon
Maintaining Healthy Operations
Schools may consider implementing several strategies to maintain healthy operations.
- Protections for Staff and Children at Higher Risk for Severe Illness from COVID-19
- Offer options for staff at higher risk for severe illness (including older adults and people of all ages with certain underlying medical conditions) that limit their exposure risk (e.g., telework, modified job responsibilities that limit exposure risk).
- Offer options for students at higher risk of severe illness that limit their exposure risk (e.g., virtual learning opportunities).
- Consistent with applicable law, put in place policies to protect the privacy of people at higher risk for severe illness regarding underlying medical conditions.
- Regulatory Awareness
- Be aware of local or state regulatory agency policies related to group gatherings to determine if events can be held.
- Gatherings, Visitors, and Field Trips
- Pursue virtual group events, gatherings, or meetings, if possible, and promote social distancing of at least 6 feet between people if events are held. Limit group size to the extent possible.
- Limit any nonessential visitors, volunteers, and activities involving external groups or organizations as possible – especially with individuals who are not from the local geographic area (e.g., community, town, city, county).
- Pursue virtual activities and events in lieu of field trips, student assemblies, special performances, school-wide parent meetings, and spirit nights, as possible.
- Pursue options to convene sporting events and participation in sports activities in ways that minimizes the risk of transmission of COVID-19 to players, families, coaches, and communities.
- Identifying Small Groups and Keeping Them Together (Cohorting)
- Ensure that student and staff groupings are as static as possible by having the same group of children stay with the same staff (all day for young children, and as much as possible for older children).
- Limit mixing between groups if possible.
- Staggered Scheduling
- Stagger arrival and drop-off times or locations by cohort or put in place other protocols to limit contact between cohorts and direct contact with parents as much as possible.
- When possible, use flexible worksites (e.g., telework) and flexible work hours (e.g., staggered shifts) to help establish policies and practices for social distancing (maintaining distance of approximately 6 feet) between employees and others, especially if social distancing is recommended by state and local health authorities.
- Designated COVID-19 Point of Contact
- Designate a staff person to be responsible for responding to COVID-19 concerns (e.g., school nurse). All school staff and families should know who this person is and how to contact them.
- Participation in Community Response Efforts
- Consider participating with local authorities in broader COVID-19 community response efforts (e.g., sitting on community response committees).
- Communication Systems
- Put systems in place for:
- Consistent with applicable law and privacy policies, having staff and families self-report to the school if they or their student have symptoms of COVID-19, a positive test for COVID-19, or were exposed to someone with COVID-19 within the last 14 days in accordance with health information sharing regulations for COVID-19external icon(e.g. see “Notify Health Officials and Close Contacts” in the Preparing for When Someone Gets Sick section below) and other applicable federal and state laws and regulations relating to privacy and confidentiality, such as the Family Educational Rights and Privacy Act (FERPA).
- Notifying staff, families, and the public of school closures and any restrictions in place to limit COVID-19 exposure (e.g., limited hours of operation).
- Put systems in place for:
- Leave (Time Off) Policies and Excused Absence Policies
- Implement flexible sick leave policies and practices that enable staff to stay home when they are sick, have been exposed, or caring for someone who is sick.
- Examine and revise policies for leave, telework, and employee compensation.
- Leave policies should be flexible and not punish people for taking time off, and should allow sick employees to stay home and away from co-workers. Leave policies should also account for employees who need to stay home with their children if there are school or childcare closures, or to care for sick family members.
- Develop policies for return-to-school after COVID-19 illness. CDC’s criteria to discontinue home isolation and quarantine can inform these policies.
- Implement flexible sick leave policies and practices that enable staff to stay home when they are sick, have been exposed, or caring for someone who is sick.
- Back-Up Staffing Plan
- Monitor absenteeism of students and employees, cross-train staff, and create a roster of trained back-up staff.
- Staff Training
- Train staff on all safety protocols.
- Conduct training virtually or ensure that social distancing is maintained during training.
- Recognize Signs and Symptoms
- If feasible, conduct daily health checks (e.g., temperature screening and/or or symptom checking) of staff and students.
- Health checks should be conducted safely and respectfully, and in accordance with any applicable privacy laws and regulations. School administrators may use examples of screening methods in CDC’s supplemental Guidance for Child Care Programs that Remain Open as a guide for screening children and CDC’s General Business FAQs for screening staff.
- Sharing Facilities
- Encourage any organizations that share or use the school facilities to also follow these considerations.
- Support Coping and Resilience
- Encourage employees and students to take breaks from watching, reading, or listening to news stories about COVID-19, including social media if they are feeling overwhelmed or distressed.
- Promote employees and students eating healthy, exercising, getting sleep, and finding time to unwind.
- Encourage employees and students to talk with people they trust about their concerns and how they are feeling.
- Consider posting signages for the national distress hotline: 1-800-985-5990, or text TalkWithUsto 66746
Preparing for When Someone Gets Sick
Schools may consider implementing several strategies to prepare for when someone gets sick.
- Advise Staff and Families of Sick Students of Home Isolation Criteria
- Sick staff members or students should not return until they have met CDC’s criteria to discontinue home isolation.
- Isolate and Transport Those Who are Sick
- Make sure that staff and families know that they (staff) or their children (families) should not come to school, and that they should notify school officials (e.g., the designated COVID-19 point of contact) if they (staff) or their child (families) become sick with COVID-19 symptoms, test positive for COVID-19, or have been exposed to someone with COVID-19 symptoms or a confirmed or suspected case.
- Immediately separate staff and children with COVID-19 symptoms (such as fever, cough, or shortness of breath) at school. Individuals who are sick should go home or to a healthcare facility depending on how severe their symptoms are, and follow CDC guidance for caring for oneself and others who are sick.
- Work with school administrators, nurses, and other healthcare providers to identify an isolation room or area to separate anyone who has COVID-19 symptoms or tests positive but does not have symptoms. School nurses and other healthcare providers should use Standard and Transmission-Based Precautions when caring for sick people. See: What Healthcare Personnel Should Know About Caring for Patients with Confirmed or Possible COVID-19 Infection.
- Establish procedures for safely transporting anyone who is sick to their home or to a healthcare facility. If you are calling an ambulance or bringing someone to the hospital, try to call first to alert them that the person may have COVID-19.
- Clean and Disinfect
- Close off areas used by a sick person and do not use these areas until after cleaning and disinfecting
- Wait at least 24 hours before cleaning and disinfecting. If 24 hours is not feasible, wait as long as possible. Ensure safe and correct use and storage of cleaning and disinfection productsexternal icon, including storing products securely away from children.
- Notify Health Officials and Close Contacts
- In accordance with state and local laws and regulations, school administrators should notify local health officials, staff, and families immediately of any case of COVID-19 while maintaining confidentiality in accordance with the Americans with Disabilities Act (ADA)external icon.
- Inform those who have had close contact with a person diagnosed with COVID-19 to stay home and self-monitor for symptoms, and follow CDC guidance if symptoms develop.
Read on cdc.gov
Parenting in a Pandemic: Tips to Keep the Calm at Home
May 18, 2020
Fear, uncertainty, and being holed up at home to slow the spread of COVID-19 can make it tough for families to keep a sense of calm. But it’s important to help children feel safe, keep healthy routines, manage their behaviorand build resilience.
Here are some tips from the American Academy (AAP) to help your family through the outbreak.
Address children’s fears
Children rely on their parents for safety, both physical and emotional. Reassure your children that you are there for them and that your family will get through this together.
- Answer questions about the pandemic simply & honestly. Talk with children about any frightening news they hear. It is OK to say people are getting sick, but say following rules like hand washing and staying home will help your family stay healthy.
- Recognize your child’s feelings. Calmly say, for example, “I can see that you are upset because you can’t have your friends over.” Guiding questions can help older children and teens work through issues. (“I know it is disappointing not to be able to hang with your friends right now. How do you think you can stay in touch with them?”)
- Keep in touch with loved ones. Children may also worry about a grandparent who is living alone or a relative or friend with an increased risk of getting COVID-19. Video chats can help ease their anxiety.
- Model how to manage feelings. Talk through how you are managing your own feelings. (“I am worried about Grandma since I can’t go visit her. The best I can do is to check in with her more often by phone. I will put a reminder on my phone to call her in the morning and the afternoon until this outbreak ends.”)
- Tell your child before you leave the house for work or essential errands. In a calm and reassuring voice, tell them where you are going, how long you will be gone, when you will return, and that you are taking steps to stay safe.
- Look forward. Tell them that scientists are working hard to figure out how to help people who get ill, and that things will get better.
- Offer extra hugs and say “I love you” more often.
Keep healthy routines
During the pandemic, it is more important than ever to maintain bedtime and other routines. They create a sense of order to the day that offers reassurance in a very uncertain time. All children, including teens, benefit from routines that are predictable yet flexible enough to meet individual needs.
- Structure the day. With the usual routines thrown off, establish new daily schedules. Break up schoolwork when possible. Older children and teens can help with schedules, but they should follow a general order, such as:
- wake-up routines, getting dressed, breakfast and some active play in the morning, followed by quiet play and snack to transition into schoolwork.
- lunch, chores, exercise, some online social time with friends, and then homework in the afternoon.
- family time & reading before bed.
A word about bedtimesChildren often have more trouble with bedtime during any stressful period. Try to keep normal nighttime routines such as Book, Brush, Bed for younger children. Put a family picture by their bed for “extra love” until morning. Bedtimes can shift some for older children and teens, but it is a good idea to keep it in a reasonable range so the sleep-wake cycle isn’t thrown off. Too little sleep makes it more challenging to learn and to deal with emotions. Remember to turn off cell phones and other mobile devices an hour before bedtime. |
|---|
Use positive discipline
Everyone is more anxious and worried during the pandemic. Younger children may not have the words to describe their feelings. They’re more likely to act out their stress, anxiety or fear through their behavior (which can, in turn, upset parents, particularly if they are already stressed). Older children and teens may be extra irritable as they miss out on time with friends and special events being cancelled.
Some ways you can help your children manage their emotions and behavior:
-
-
- Redirect bad behavior. Sometimes children misbehave because they are bored or don’t know any better. Find something else for them to do.
- Creative play. Suggest your children draw pictures of ways your family is staying safe. Make a collage and hang it up to remind everyone. Or, build an indoor fort or castle to keep the germs at bay, bringing in favorite stuffed animals or toys.
- Direct your attention. Attention–to reinforce good behaviors and discourage others–is a powerful tool. Notice good behavior and point it out, praising success and good tries. Explaining clear expectations, particularly with older children, can help with this.
- Use rewards & privileges to reinforce good behaviors (completing school assignments, chores, getting along with siblings, etc.) that wouldn’t normally be given during less stressful times.
- Know when not to respond. As long as your child isn’t doing something dangerous and gets attention for good behavior, ignoring bad behavior can be an effective way of stopping it.
- Use time-outs. This discipline tool works best by warning children they will get a time-out if they don’t stop. Remind them what they did wrong in as few words―and with as little emotion―as possible. Then, remove them from the situation for a pre-set length of time (1 minute per year of age is a good guide).
-
Special Time InEven with everyone home together 24/7, set aside some special time with each child. You choose the time, and let your child choose the activity. Just 10 or 20 minutes of your undivided attention, even if only once every few days, will mean a lot to your child. Keep cell phones off or on silent so you don’t get distracted. |
|---|
- Avoid physical punishment. Spanking, hitting, and other forms of physical or “corporal” punishment risks injury and isn’t effective. Physical punishment can increase aggression in children over time, fails to teach them to behave or practice self-control, and can even interfere with normal brain development. Corporal punishment may take away a child’s sense of safety and security at home, which are especially needed now.
| The AAP reminds parents and caregivers never to shake or jerk a child, which could cause permanent injuries and disabilities and even result in death. Tips for calming a fussy baby and advice for caregivers who have reached a breaking point can be found here. If you have a friend, relative, or neighbor with the new baby at home, think of ways you can reach out to provide support during the isolation period. |
|---|
- Take care of yourself. Caregivers also should be sure to take care of themselves physically: eat healthy, exercise and get enough sleep. Find ways to decompress and take breaks. If more than one parent is home, take turns watching the children if possible.
- Remember to take a breath. In addition to reaching out to others for help, the AAP recommends parents feeling overwhelmed or especially stressed try to take just a few seconds to ask themselves:
- Does the problem represent an immediate danger?
- How will I feel about this problem tomorrow?
- Is this situation permanent?
In many cases, the answers will deflate the panic and the impulse to lash out physically or verbally at children.
Read on healthychildren.org
Cloth Face Coverings for Children During COVID-19
May 18, 2020
To protect ourselves and others from COVID-19, the CDC now recommends cloth face coverings be used when outside. But what about children? Read on for answers to some frequently asked questions about cloth face coverings and children during the COVID-19 pandemic.
Why are people wearing cloth face coverings right now?
Since so many people who have COVID-19 don’t have symptoms, wearing cloth face coverings reduces the chance of transmitting the virus through the spray of spit or respiratory droplets. This is especially true for when someone with COVID-19 comes within 6 feet of you, which is the range of transmitting infection through acts like sneezing or coughing.
Should children wear cloth face coverings?
Children under the age of 2 years should not wear cloth face coverings.
When do children need to wear cloth face coverings?
There are places where children should wear cloth face coverings. This includes places where they may not be able to avoid staying 6 feet away from others. For example, if you have to take them to the doctor, pharmacy, or grocery store.
However, there are other places where children do NOT need to wear a cloth face covering:
- At home, assuming they have not been exposed to anyone with COVID-19.
- Outside, as long as they can stay at least 6 feet away from others and can avoid touching surfaces. For example, it’s fine to take a walk as long as your children stay 6 feet away from others and do not touch tables, water fountains, playground equipment or other things that infected people might have touched.
Caution: you may need to reconsider the use of cloth face coverings if:
- The face coverings are a possible choking or strangulation hazards to your child.
- Wearing the cloth face covering causes your child to touch their face more frequently than not wearing it.
Staying home and physical distancing is still the best way to protect your family from COVID-19. Especially for younger children who may not understand why they can’t run up toward other people or touch things they shouldn’t, it’s best to keep them home.Children who are sick (fever, cough, congestion, runny nose, diarrhea, or vomiting) should not leave home.
What if my child is scared of wearing a face covering?
It’s understandable that children may be afraid of cloth face coverings at first. Here are a few ideas to help make them seem less scary:
- Look in the mirror with the face coverings on and talk about it.
- Put a cloth face covering on a favorite stuffed animal.
- Decorate them so they’re more personalized and fun.
- Show your child pictures of other children wearing them.
- Draw one on their favorite book character.
- Practice wearing the face covering at home to help your child get used to it.
For children under 3, it’s best to answer their questions simply in language they understand. If they ask about why people are wearing cloth face coverings, explain that sometimes people wear them when they are sick, and when they are all better, they stop wearing them.
For children over 3, try focusing on germs. Explain that germs are special to your own body. Some germs and good and some are bad. The bad ones can make you sick. Since we can’t always tell which are good or bad, the cloth face coverings help make sure you keep those germs away from your own body.
One of the biggest challenges with having children wear cloth face coverings relates to them “feeling different” or stereotyping them as being sick. As more people wear these cloth face coverings, children will get used to them and not feel singled out or strange about wearing them.
What about children with special health care needs?
- Children who are considered high-risk or severely immunocompromised are encouraged to wear an N95 mask for protection.
- Families of children at higher risk are encouraged to use a standard surgical mask if they are sick to prevent the spread of illness to others.
- Children with severe cognitive or respiratory impairments may have a hard time tolerating a cloth face covering. For these children, special precautions may be needed.
Is there a “right way” to wear a cloth face covering?
Yes. Place the cloth face covering securely over the nose and mouth and stretch it from ear to ear. Remember to wash your hands before and after you wear it and avoid touching it once it’s on your face. When back inside, avoid touching the front of the face covering by taking it off from behind. Cloth face coverings should not be worn when eating or drinking.
Wash cloth face coverings after each wearing.
What kind of cloth face covering is best?
Homemade or purchased cloth face coverings are fine for most people to wear. For children, the right fit is important. Pleated face coverings with elastic are likely to work best for kids. Adult cloth face coverings are usually 6×12 inches, and even a child-sized 5×10 inch covering may be too large for small children. Try to find the right size for your child’s face and be sure to adjust it for a secure fit.
Due to very limited supply now, professional grade masks like N-95 masks should be reserved for medical professionals on the front lines who have increased risk of exposure to coronavirus.
Read on healthychildren.org
Tips for Coping with a New Baby During COVID-19
May 18, 2020
All babies cry. Most babies cry a lot from two weeks to two months of age. Some cry more than others, and some cry longer than others. For many new parents, crying is one of the most stressful parts of coping with a newborn.
In some cases, extreme stress and a temporary lapse of emotional control in a caregiver can lead to actions that result in abusive head trauma. In fact, the most common trigger for abusive head trauma is simply a crying baby. The American Academy of Pediatrics released a policy statement on the medical aspects of abusive head trauma and points out that actions that lead to abusive head trauma are often the result of when caretakers experience stress and get to the end of their rope.
However, there is a bright side: The key to preventing actions that lead to abusive head trauma is to understand how common feelings of frustration, isolation, and exhaustion are during the first few months of an infant’s life.
Helpful tips
Usually, new parents can seek out social supports and external help—but what happens now, when we are all restricted in our movements and our contacts? What happens when grandparents can’t come over to help out, or when neighbors don’t stop by for a cup of coffee? What happens when families are hit with sudden job loss, loss of childcare, and other restrictions resulting from the COVID-19 pandemic? Here are a few suggestions:
- Try all the soothing tricks. Crying babies want to be soothed. You may need to try a few things, over and over, before they calm. Try holding them, feeding them, swaddling them, gently rocking them, singing to them. If these don’t work, put the baby down and take a break. Be sure your baby is in a safe sleep environment (on their back on a firm sleep surface with a tight-fitting sheet, away from soft blankets, toys, pillows, and other bedding materials). While some babies cry for a long time, many parents are surprised at how rapidly babies will cry themselves to sleep.
- Pay attention to your own needs. The challenges of new mothers can certainly feel overwhelming sometimes. Rest as much as you can—try sleeping when the baby does. Find time for yourself when your partner or other caring adult watches the baby. Put on your headphones, give a friend or relative a call, have a cup of tea, or just relax.
- Connect with others. Social distancing during the COVID-19 outbreak can be isolating. Try video chats or social media to stay in touch. If you’re a friend or relative on the receiving end of these calls, listen first before offering suggestions. Imagine you are with the young parent, they are crying on your shoulder, and you are offering reassurance without any words. Keeping this image in mind can help you provide the social support that all new parents need.
- Use your “helpers.” Engage older siblings as much as you can by encouraging them to be your special helpers, so they can help out in developmentally appropriate ways.
- Seek help. Depression is the most common mental illness in the United States. If you had a history of depression before your baby was born, you may be at higher risk for postpartum depression. Speak with your provider sooner rather than later to help foresee this potential condition. Many doctors, nurses, and mental health providers are now set up for telehealth visits and may be able to help you by video or phone.
- Reach out. If you are a friend, relative, or neighbor to a family with a newborn, this is the time to reach out. Think about ways you can help. In addition to social support, can you buy diapers or other baby supplies? Can you drop off food or treats for the siblings or adults? Can you safely supervise older children outdoors? Maybe they could come along with you when you walk your dog!
- Help a co-worker out. If you are a co-worker of a parent returning to work (especially during social distancing) after parental leave, be kind and supportive. If you see or hear the baby on the call, say Hi!
- Find a forum. New mothers may find it helpful to discuss their experiences with other new mothers. In addition to seeking help from friends, relatives, neighbors, and medical professionals, look for discussion forums and communities of moms dedicated to sharing problems, stories, and tips with each other online (see the list of resources below).
- Your pediatrician is here to help. Never hesitate to call for advice. Your pediatricians is an excellent resource for understanding your baby and your own needs, including those related to postpartum depression.
- Resources. Here are a few key resources that may be helpful to you at home:
- All Babies Cry offers tips and suggestions for parents of newborns.
- The University of Colorado has stress relief tips during this period of isolation.
- Prevent Child Abuse America has tips and resources for parents, children, and others.
- Postpartum Support International toll-free Help Line, in English and Spanish, refers callers to appropriate local resources: 1-800-944-4773 or text 1-503-894-9453 (English) or 1-971-420-0294 (Spanish)
- Smart Patients Postpartum Community: online community of peer support and active discussion forums.
- The Office on Women’s Health has information to support breastfeeding mothers.
Read on healthychildren.org By: Robert Sege, MD, PhD, FAAP
Expect more cases of strange coronavirus syndrome in kids, doctors warn
May 14, 2020
Parents, hospitals and clinics should expect to see more cases of a mystifying condition that seems to be affecting children after a bout with Covid-19, doctors said Wednesday.
The condition, called multisystem inflammatory syndrome in children, appears to be a post-viral syndrome, said Dr. Jeffrey Burns, a critical care specialist at Boston Children’s Hospital who has been coordinating a global group of doctors who compare notes on the condition.
Doctors are investigating cases in at least 150 children, most of them in New York. But a CNN survey finds hospitals and clinics in at least 17 states and Washington, DC are checking into suspected cases.
“This multisystem inflammatory syndrome is not directly caused by the virus,” Burns told CNN. “The leading hypothesis is that it is due to the immune response of the patient.”
Symptoms include persistent fever, inflammation and poor function in organs such as the kidneys or heart. Children may also show evidence of blood vessel inflammation, such as red eyes, a bright red tongue and cracked lips, said Dr. Moshe Arditi, a pediatric infectious diseases expert at Cedars-Sinai Medical Center in Los Angeles.
Dr. Ngozi Ezike, director of the Illinois Department of Public Health, said it’s a complicated disorder.
“It’s a spectrum of disorders, and so in some cases you’ll have the individual have coronary artery involvement. Sometimes they don’t,” Ezike told a news conference.
A delayed response to infection
Not all of the affected children have tested positive for the coronavirus, but reports from Europe and from several cities in the United States show a link.
“There seems to be delayed responses to Covid infections in these kids,” Arditi said.
Burns believes more cases will turn up as Covid-19 affects more people. It’s a rare condition, but rare consequences of viral infections are seen more often when millions of people are infected.
“We can expect that each of the epicenters will see clusters of these emerging roughly four to six weeks later,” Burns told CNN.
“It makes sense that it emerged in New York first because New York had the largest and most severe outbreak (of Covid-19), followed by New Jersey and, unfortunately, Boston.”
Most children are not seriously affected by the syndrome, Burns said. Most don’t even need treatment in the intensive care unit, he said, although a very few have died. “We do have proven treatments that we can use and are using,” he said. They include blood thinners and immune modulators.
The Centers for Disease Control and Prevention is preparing a Health Alert Network notification to send to doctors across the country, a CDC spokesman said. Burns said the World Health Organization is also working to define the syndrome and alert doctors so they will know what to look for and how to treat it.
“This new entity has some similarities to Kawasaki disease,” Arditi told CNN. “But there are a lot more features that are consistent with toxic shock syndrome, such as multi-organ system involvement and severe abdominal involvement with diarrhea,” he added.
It will be important to study, because the response could help explain why children are so much less likely to be severely affected by Covid-19 than adults are, said Burns.
“Understanding the child’s immune response could be a key to vaccine development and could also be a key to therapy for adults to understand why children are able to fight (Covid-19) off so well,” Burns said.
Doctors find suspected cases in 17 states
CNN has contacted departments of health, hospitals and state officials around the country to get a sense of how many children are affected, and where.
Some state health departments told CNN that they are waiting for the CDC alert. “We are working with the CDC on a case definition and are looking into possible cases, but won’t have more until the CDC finalizes its definition,” a spokesman for the Minnesota Department of Health said.
“We don’t believe this syndrome is very common, but several cases have been reported elsewhere in association with Covid-19,” said Dr. Paul Cieslak, medical director for infectious diseases and immunizations at the Oregon Health Authority Public Health Division. “This syndrome appears to be an uncommon but serious complication of Covid-19 in children.”
Paul Mounds, chief of staff for the Connecticut governor’s office, said the syndrome would be trackable illness in the state. The Department of Public Health “sent this out to all the Connecticut pediatric health systems to make sure that they are reporting if these cases are occurring in their facilities, so we can be able to track it and handle it accordingly,” Mounds said Wednesday.
States reporting cases include:
- California
- Delaware
- Illinois
- Kentucky
- Louisiana
- Massachusetts
- Michigan
- Minnesota
- Missouri
- New Jersey
- New York
- Ohio
- Oregon
- Pennsylvania
- Tennessee
- Utah
- Washington
Read on Apple News
COVID-19 and Pediatric Multi-System Inflammatory Syndrome
May 13, 2020
You may have heard news reports about a possible connection between COVID-19 and a serious health condition in children currently called Pediatric Multi-system Inflammatory Syndrome (sometimes called PIMS). We are watching this very carefully and trying to learn all that we can about it. Scientists around the world are working hard to understand this syndrome and how best to treat it.
Until then, we want to reassure parents that most children are not affected by the coronavirus, and reports of children who become seriously ill remain rare and unusual cases.
What we know
Despite being rare, there are reports of some children getting sick – whether from COVID-19 or from other causes, including PIMS. Some of these children reported to have this condition have tested positive for COVID-19, while others have not.
This is why it is so important that you call your pediatrician if you have anyconcerns about your child’s health. Pediatricians are open for business and able to care for your children now.
Symptoms
You may have heard it compared to other rare childhood conditions such as Kawasaki Disease or Toxic Shock Syndrome, but at this time, it is thought to be a separate condition.
If you notice any of the following symptoms, call your pediatrician:
- a fever that won’t go away
- abdominal pain, diarrhea or vomiting
- rash or changes in skin color
- trouble breathing
- your child seems confused or overly sleepy
Your pediatrician will let you know if your child needs to be seen in the office or if you need to go to the emergency department.
While Pediatric Multi-system Inflammatory Syndrome sounds frightening, the American Academy of Pediatrics reminds parents that this condition is very rare.
Remember
Call your pediatrician if you have any questions or concerns about your child. Do not be afraid to go to the pediatrician’s office for checkups, vaccines, or if your child is sick. Your pediatrician cares about your child’s health and is taking extra steps to make sure everyone is safe when they come in.
Read on healthychildren.org
Chesterfield Health District hosting free COVID-19 testing for the uninsured
May 12, 2020
CHESTERFIELD COUNTY, Va. – The Chesterfield Health Department is hosting free COVID-19 testing this week for uninsured or underinsured residents of the Chesterfield Health District, which includes the counties of Chesterfield and Powhatan and the City of Colonial Heights.
The testing is part of a statewide push to increase testing across the commonwealth, particularly for low-income and uninsured Virginians.
The free testing is being offered for people who have COVID-19 symptoms and who may not have insurance, or whose insurance does not cover COVID-19.
Testing will take place this week at the following locations:
Wednesday, May 13 at 9 a.m.
Greenleigh Mobile Home Park
14006 Stevenhurst Drive
Friday, May 15 at 9 a.m.
Bellwood Drive-In/Flea Market
9201 Jefferson Davis Highway
Spanish speaking staff will be present during the testing events.
Health officials urge residents to make an appointment prior to arrival. While some appointments will be reserved for walk-ups that morning, testing is limited.
Residents who may be experiencing COVID-19 symptoms as defined by the CDC, is asked to call the Chesterfield Health Department at 804-318-8207 to make an appointment.
Read on WTVR Channel 6
CDC Recommendations Regarding Cloth Face Covering
May 6, 2020
Use of Cloth Face Coverings to Help Slow the Spread of COVID-19
Coronavirus Self Checker
April 28, 2020
A guide to help you make decisions and seek appropriate medical care: Coronavirus Self Checker
These are the 6 new possible symptoms of the coronavirus the CDC added to its list
April 28, 2020
Chills, repeated shaking with chills, muscle pain, headache, sore throat and a loss of taste or smell are the new symptoms added to the CDC list.
Read in USA TODAY
Designated Well/Sick Offices and Appointment Changes
March 15, 2020
Please be advised, beginning Wednesday, March 18, 2020 we are temporarily changing our operating procedures. The Midlothian Village office will be a sick clinic only. Sick visits will not be seen at the Bon Air or Powhatan offices.
All wellness visits will be scheduled at the Bon Air and Powhatan offices. This includes routine check-ups, medication checks and consultations. All lactation visits will be scheduled at the Bon Air office. If you have one of the aforementioned appointments scheduled between March 18, 2020 and March 31, 2020 at the Midlothian Village office, we will call you to reschedule. We will have specific clinic teams working at well and sick offices. They will not be rotating between sick and well designated offices. This is in effort to minimize potential exposure of COVID-19 to patients and staff. Therefore, it is possible you may not see the provider originally scheduled for a wellness visit. We will begin contacting impacted patients Monday March 16, 2020.
As is currently recommended by the Virginia Department of Health, we will provide phone triage screening and recommendations that may include referring potentially exposed patients to a COVID-19 Testing Center. Any child with symptoms and known, or potential exposures, to COVID-19 will not be evaluated in our offices.
To ensure a highly sanitary environment, our wait rooms will be rigorously disinfected throughout the day at scheduled intervals. Additionally, patients with sick visit appointments are welcome to call 804-794-2821 to check-in upon arrival to the Midlothian Village office and wait in their car until the nurse has an available exam room available.
We apologize for any inconveniences these changes may cause. This is a fluid situation subject to change as new information becomes available. We will continue to follow the recommendations of the CDC and VDH and share updates as they impact our patients and operating procedures.
COVID-19 (Coronavirus) Patient safety update
March 13, 2020
1) 1 patient, 1 parent/guardian. When possible, we ask that only the patient and one parent/guardian come to the office for sick or well visits. We understand that due to childcare availability and other challenges this may not always be possible, however, when possible this is a practical way of minimizing potential or unnecessary exposures.
2) All books, magazines and toys will be removed from our waiting rooms. Please feel free to bring your own activities to keep your child occupied.
3) We are following the guidelines and recommendations of the CDC, VDH and AAP. We have also implemented additional precautions and safeguards to ensure the safety and well-being of our patients. At this time, we are not rescheduling any previously scheduled well-child examinations, medication checks and/or consultations, however, if your child has any illness symptoms on the day of their check-up, please call us before your appointment so that we may appropriately triage.
4) When CALLING for a sick visit please be prepared to answer a series of YES or NO questions regarding symptoms AND possible exposure. If you know or believe your child has been exposed to COVID-19, if your child has been in contact with someone who has COVID-19, has been formally tested for COVID-19, or is suspected of having COVID-19, this MUST be disclosed so that we may provide appropriate support and guidance.
>>> Health department sets up 1st COVID-19 pop-up testing site at Dorey Park in Henrico County.
>>> Federal officials warn against coronavirus scams targeting most vulnerable.

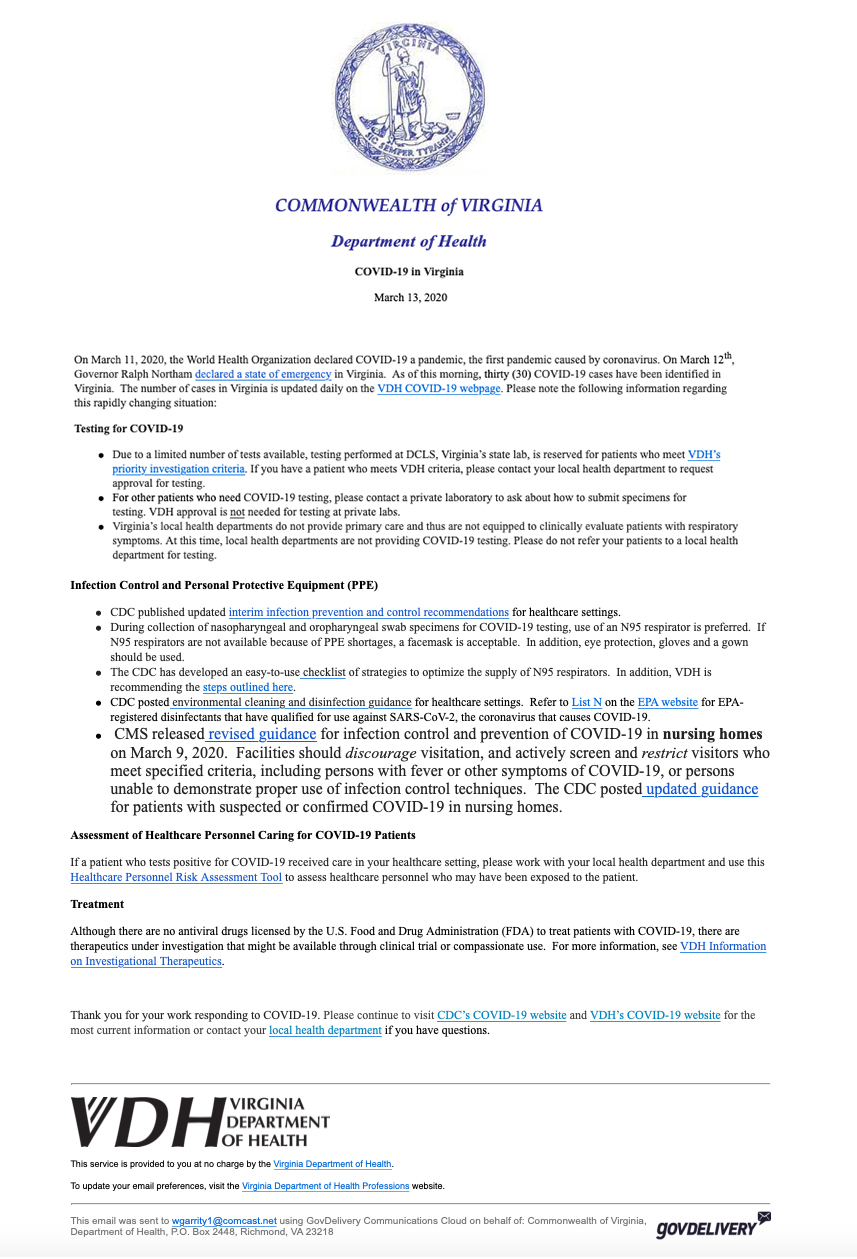
COVID-19 information from Virginia Department of Health
Additionally, we recommend the following websites as resources:
VCU Health Coronavirus Hotline: 804-628-7425
https://www.cdc.gov/coronavirus/2019-ncov/about/index.html
https://www.chrichmond.org/blog/coronavirus-what-you-need-to-know
http://www.vdh.virginia.gov/surveillance-and-investigation/novel-coronavirus/
https://www.washingtonpost.com/lifestyle/2020/03/14/parenting-tips-coronavirus/












 Andrea Gordon, M.D., FAAP
Andrea Gordon, M.D., FAAP













Recent Comments